What is TTP?
Thrombotic thrombocytopenic purpura (TTP) is a rare blood disorder1
TTP is a rare condition that causes small blood clots in blood vessels throughout your body.
Normal blood flow
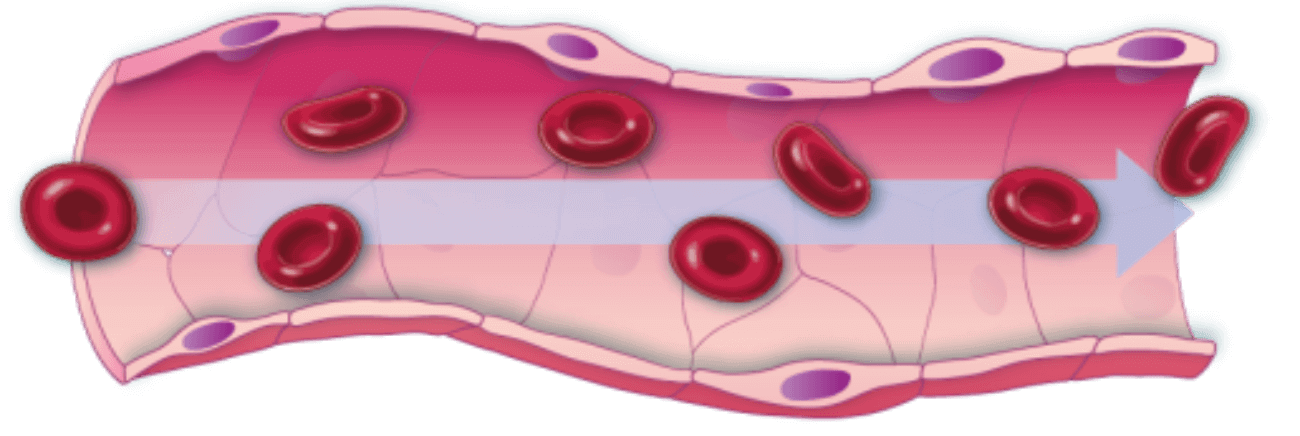
Blood vessels are tubes that carry blood through your body. A blood clot is a clump of blood cells, called platelets, that are stuck together. Normally, platelets float in your blood and form clots only when you need them to help you stop bleeding.
Blood clot in TTP
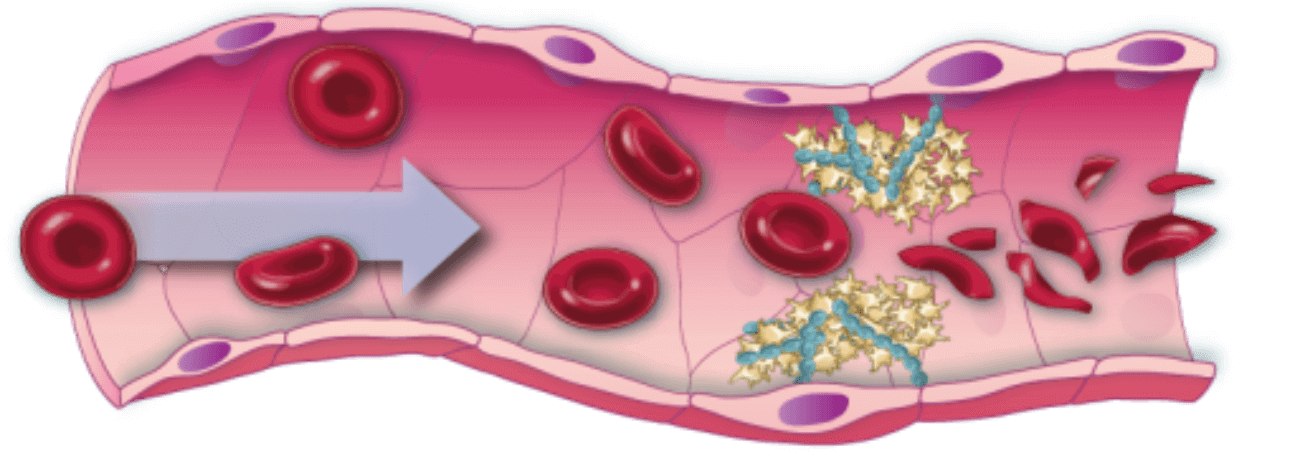
When you have TTP, platelets make clots when they’re not supposed to in a blood vessel. This makes it hard for blood to move through the blood vessel to get to the rest of your body.
When clots from TTP make it hard for blood to move through your body the right way, it can cause serious health problems like:
-
Bleeding underneath the skin (bruising)
-
Not having enough platelets in your blood to make the clots your body actually needs (to help you stop bleeding)
-
Damage to the red blood cells, which carry oxygen through your body
-
Organ dysfunction that can result in serious events like seizures, heart attacks, or strokes
Learn more about what happens in your body when you have TTP.
Breaking down the words “thrombotic thrombocytopenic purpura”
The words that make up TTP help explain what is happening in your body.
THROMBOTIC means blood clots form in the blood vessels.
THROMBOCYTOPENIC means having a lower number of blood platelets than you should. This happens because the platelets are clumping together to make the clots in your blood vessels.
PURPURA are purple bruises that are caused by bleeding under your skin. These bruises are a key symptom of TTP.
TTP also causes more serious symptoms.
So THROMBOTIC THROMBOCYTOPENIC PURPURA means that something is happening in your body to make clots form in your blood vessels. These clots cause key TTP symptoms, like a low number of platelets in your blood and purple bruises.
What causes TTP?1,2
There are 2 types of TTP, acquired and hereditary. Acquired TTP is caused by a problem in your immune system. Hereditary TTP is caused by a problem in a gene passed down through your family. Both types of TTP lead to not having enough of a protein called ADAMTS13 in your blood. ADAMTS13 helps your blood flow normally and clot only when your body needs it.
Types of TTP
Acquired TTP2-5
(also called immune-mediated TTP)
- The most common form of TTP
- Caused by a problem in the immune system that results in low levels of ADAMTS13 in the blood
- Often develops in adulthood
- Usually diagnosed because of a serious health problem (this is considered the first TTP episode)
Hereditary TTP3,6,7
(also called congenital, inherited, or familial TTP)
- A very rare form of TTP
- Caused by a problem in a gene that is passed down through families and results in low levels of ADAMTS13 in the blood
- Often develops in early childhood
- Usually diagnosed early because the person doesn’t have enough ADAMTS13 in their blood when they are born
TTP is rare, unpredictable, and causes blood clots.3
The cause of acquired TTP is unknown, but there may be triggers1,8-10
The majority of TTP cases are acquired, but it’s not fully understood why people develop TTP as adults. This can be very frustrating, especially when you want to understand how or why you have this condition. While there are no clear reasons why someone will acquire TTP, certain things might jump-start the problem in the immune system. These are often called “triggers.”
Potential TTP triggers
Personal health conditions, including cancer, HIV, and lupus
Certain treatments and/or medicines
Infections
Pregnancy
Are you or someone you love in the hospital with TTP?
Who is affected by TTP?5,11,12
TTP can affect anyone, but it is more common in some groups of people than in others.
People are usually between
years old when they have their first TTP episode
Women make up
of people with TTP
Black people are
more likely to have TTP than people who are not Black
Learn what happens in your body when you have TTP.
Medical history, symptoms, and blood tests all help to diagnose TTP.
References: 1. Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood. 2017;129(21):2836-2846. doi:10.1182/blood-2016-10-709857 2. Scully M, Cataland SR, Peyvandi F, et al. N Engl J Med. 2019;380(4):335-346. doi:10.1056/NEJMoa1806311 3. Zheng XL, Vesely SK, Cataland SR, et al. ISTH guidelines for the diagnosis of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020;18(10):2486-2495. doi:10.1111/jth.15006 4. Reese JA, Muthurajah DS, Kremer Hovinga JA, Vesely SK, Terrell DR, George JN. Children and adults with thrombotic thrombocytopenic purpura associated with severe, acquired Adamts13 deficiency: comparison of incidence, demographic and clinical features. Pediatr Blood Cancer. 2013;60(10):1676-1682. doi:10.1002/pbc.24612 5. Sukumar S, Lämmle B, Cataland SR. Thrombotic thrombocytopenic purpura: pathophysiology, diagnosis, and management. J Clin Med. 2021;10(3):536. doi:10.3390/jcm10030536 6. Congenital thrombotic thrombocytopenic purpura. NIH Genetic and Rare Diseases Information Center website. Updated July 12, 2018. Accessed December 3, 2021. https://rarediseases.info.nih.gov/diseases/9430/congenital-thrombotic-thrombocytopenic-purpura 7. George JN, Cuker A. Hereditary thrombotic thrombocytopenic purpura (TTP). UpToDate website. Updated August 22, 2021. Accessed December 3, 2021. https://www.uptodate.com/contents/hereditary-thrombotic-thrombocytopenic-purpura-ttp 8. Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91(1):1-19. doi:10.1007/s12185-009-0476-1 9. Goel R, King KE, Takemoto CM, Ness PM, Tobian AAR. Prognostic risk-stratified score for predicting mortality in hospitalized patients with thrombotic thrombocytopenic purpura: nationally representative data from 2007 to 2012. Transfusion. 2016;56(6):1451-1458. doi:10.1111/trf.13586 10. Stylianou K, Tsirakis G, Mantadakis E, et al. Refractory thrombotic thrombocytopenic purpura associated with oral contraceptives and factor V Leiden: a case report. Cases J. 2009;2:6611. doi:10.1186/1757-1626-2-6611 11. Terrell DR, Williams LA, Vesely SK, Lämmle B, Hovinga JAK, George JN. The incidence of thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: all patients, idiopathic patients, and patients with severe ADAMTS-13 deficiency. J Thromb Haemost. 2005;3(7):1432-1436. doi:10.1111/j.1538-7836.2005.01436.x 12. Azoulay E, Bauer PR, Mariotte E, et al; Nine-i Investigators. Expert statement on the ICU management of patients with thrombotic thrombocytopenic purpura. Intensive Care Med. 2019;45(11):1518-1539. doi:10.1007/s00134-019-05736-5
