What happens in your body when you have TTP?
Thrombotic thrombocytopenic purpura (TTP) causes clots in your blood vessels1-4
TTP is a complicated condition. It causes small blood clots in small blood vessels. These clots can cause serious problems if they are not treated quickly.
What happens in the blood normally
Blood is made up of many different parts, also called components. Some of these components help the blood flow normally, while some help make clots. Clots are clumps of blood that are stuck together. Usually, blood clots are made because your body needs them for something, like to help you stop bleeding if you cut yourself.
To understand TTP, it helps to understand 3 important components of the blood
Platelets
A component of your blood that helps create clots when your body needs them. When you cut yourself, platelets (small blood cells) help your body form clots to stop bleeding.
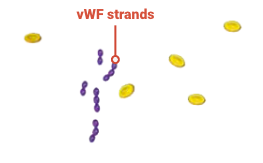
von Willebrand factor (vWF)
A component of your blood that can form long strands and attach to platelets. It helps the platelets stick together to form a clot and stop bleeding.
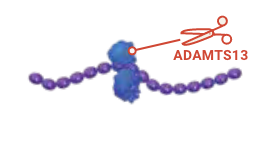
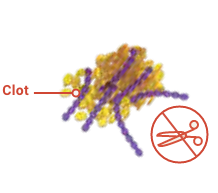
ADAMTS13
A helpful protein in the blood that keeps vWF strands from getting too long. ADAMTS13 finds vWF strands and clips them into little pieces. Essentially, ADAMTS13 makes vWF strands the right size to make the right amount of platelets stick.
In people with acquired TTP, 3 key things happen in the blood
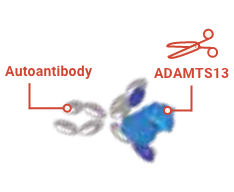
The immune system mistakenly attacks ADAMTS13.
The immune system wrongly creates autoantibodies that attack ADAMTS13. Because of this, there is not enough ADAMTS13 in the blood.
Without ADAMTS13, vWF strands grow out of control.
The strands of vWF become too long and lots of platelets stick to the strands.
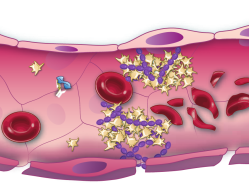
Together, platelets and vWF form dangerous clots, often in your smaller blood vessels.
These clots can cause serious heath problems if not treated quickly.
Blood clots from TTP have serious risks
• Make it hard for blood to move through the blood vessels to the rest of your body. This can cause serious problems like stroke, heart attack, or organ damage
• Cause anemia. This means there aren’t enough red blood cells in your blood. Since red blood cells carry oxygen, not having enough of them means not enough oxygen is being carried through your body
• Lower the number of platelets in the blood. This can lead to problems like not being able to stop cuts from bleeding, bruising, and bleeding inside your body
Because blood clots from TTP can cause serious problems, they need treatment as soon as possible. The longer clots go untreated, the higher the risk of serious health problems.
Even though TTP is serious, it can be treated.
There are different treatments available to help each problem happening in the blood. Talk with your healthcare team about all the available treatments for TTP.
The main problem in TTP is that there is not enough ADAMTS13 in the blood.
There are treatments recommended by experts to help each problem in the blood.
TTP can be managed, but it’s important to watch out for episodes.
References: 1. Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91(1):1-19. doi:10.1007/s12185-009-0476-1 2. Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood. 2017;129(21):2836-2846. doi:10.1182/blood-2016-10-709857 3. Scully M, Hunt BJ, Benjamin S, et al; British Committee for Standards in Haematology. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323-335. doi:10.1111/j.1365-2141.2012.09167.x 4. Goel R, King KE, Takemoto CM, Ness PM, Tobian AAR. Prognostic risk-stratified score for predicting mortality in hospitalized patients with thrombotic thrombocytopenic purpura: nationally representative data from 2007 to 2012. Transfusion. 2016;56(6):1451-1458. doi:10.1111/trf.13586
